Making the most of patient experience data
Patient experience data has long been used as a measure of quality of healthcare, but there remains a gap between measurement and improvement. The ethnographic study by Locock et al [1] “Understanding how frontline staff use patient experience data for service improvement”, evaluated whether and how NHS staff used patient experience information. The focus of this study was on understanding how staff approached patient experience projects, why some struggled, and how they made sense of the tasks.
What can be applied from the findings of this study to make more use of patient experience data?
What was the research?
Locock et al documented how frontline hospital ward teams engaged with patient experience data, what challenges they faced and how they could be better supported to work on person-centred quality improvement.
The year-long ethnographic study was conducted in six medical wards at different hospital sites in the UK. In every site, staff undertook quality improvement projects using a range of data sources.
What is patient experience data?
Most people understand patient experience data to be feedback from surveys and this does make a significant contribution. However, there is also ‘soft’ intelligence that can be seen as expressions of patient feedback. This can range from patients’ stories, ‘thank you’ cards, informal comments and observations that provide insight into ward-specific patient experience.
Locock et al found that staff knew of issues and were responding, without being able to identify any specific piece of patient feedback. In some cases, such staff-initiated improvements were backed up by formal patient experience data.
When is the data used most successfully?
The research team found that when hospital teams combined a range of staff from different professions, they generated a higher level of quality improvement than those adopting a single disciplinary approach. The staff did not necessarily need to be senior or from a particular profession to drive change. When the Patient Experience Office was included in projects there tended to be more ambitious improvement activities being addressed. This may have been because the Patient Experience Office was able to help by using their data knowledge and insight to add to the project.
A study by Sheard et al [2] focussed on the ward teams’ engagement with patient feedback. This study found three components were needed to effect change:
1) The staff’s belief in the importance of responding to feedback and wanting to act.
2) The staff believing they had sufficient ownership, autonomy and resources to establish an action plan.
3) Management support for the team to work on improvement and the capacity to collaborate with other departments.
What were the challenges?
Locock et al noted a range of challenges faced by the researchers in engaging staff to use patient experience data. These included:
- Logistical issues – Quiet space for staff to meet and sustainable funds for minor improvements.
- Encouraging staff empathy and creativity to improve patient experience without assuming that staff always know best.
- Whether organisations recognised specific forms of patient experience information as ‘data’ had a legitimising effect and influenced whether the staff felt the data was actionable.
- Developing the knowledge to utilise information from patient stories and free-text feedback in surveys.
- Lack of organisational support to use feedback from social media at ward-level prevented the project team from being engaged with it.
- Staff were receptive to and motivated by positive feedback from patients, but did not tend to see this as a source of ideas for quality improvement.
- Negative feedback, though useful, could be difficult for staff to accept and could prevent efforts at improvement.
- Teams with a more restricted range of staff involved and those with a more distant relationship with the Patient Experience Office faced greater challenges.
Key learnings
Locock et al suggested that establishing a network of individuals with assorted levels of Bourdieu’s [3] four forms of capital: economic, social, symbolic and cultural (see Table 1) is a key mechanism for achieving person-centred improvement in the NHS.
Table 1
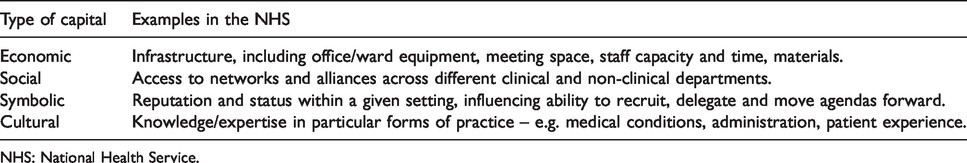
Having a varied team with different knowledge and skills generates more practical, organisational and social resources to drive change. The report particularly recommended that those working on patient experience projects seek to include hands-on frontline staff, in addition to authoritative figures.
Where to look for more help
Locock et al have produced an open-access guide to using patient experience data and incorporated it into face-to-face training courses led by the Point of Care Foundation.
For more information about the use of patient experience data in the NHS read the NIHR’s review.
This research was funded by the National Institute for Health Research (NIHR) under its Health Services and Delivery Research Programme (14/156/06). The views expressed are those of the authors, and not necessarily those of the NHS, the NIHR or the Department of Health.
References
[1] Locock L, et al. Understanding how frontline staff use patient experience data for service improvement: an exploratory case study evaluation, 2020.
[2] Sheard et al. The Patient Feedback Response Framework – Understanding why UK hospital staff find it difficult to make improvements based on patient feedback: A qualitative study, 2017.
[3] Bourdieu P. Distinction: a social critique of the judgement of taste. London, UK: Routledge and Kegan Paul, 1984.

