Where does person centred care fit in when dealing with pandemics?
For more than 70 years, we have come to expect that the National Health Service (NHS) is always there for us when we need it. It has been a source of comfort to many that should anyone become ill the NHS is available, free at point of contact, offering equitable and normally high quality medical care. COVID-19 has required the nation to lean even more on its health service; whilst most of us are locked down at home, key workers are keeping the country running.
This year is Picker’s 20th anniversary as an independent charity. Throughout the last 20 years, we have worked to influence, inspire, and empower the delivery of the highest quality person centred care for all, always. We’ve pioneered new methods of understanding and measuring people’s experiences of care and popularised the term “person centred care”; where an individuals’ personal needs and requirements are an integral part of planning their care (for patients), or working environment (for staff).
The benefits of person centred care are clear. Actively involving people in their care, treatment and support improves outcomes and provides a better experience for patients as well as producing cost savings. Similarly, research shows that when health and social care staff are happy, they work more efficiently and take less time off work with stress-related illnesses. The results of this are improved patient care and reduced costs from employing agency staff to cover sick leave and empty posts.
However, with the arrival of COVID-19 comes many new challenges. Health and social care staff are now so stretched that we’ve had to call back retired medics; it’s not unusual for staff to live away from their families for fear of bringing the virus home; and we have volunteers covering some positions. At times like this, should person centred care be considered more luxury than necessity?
It is tempting to argue that the proper response to a crisis should be to pare back services to their most fundamental elements: to focus singularly on clinical care. But every care episode, every treatment, is at its most basic a personal interaction – and even under the greatest stress we should strive to keep patients at the centre of services. The benefits of providing high quality person centred care still exist and it could be argued are now more important than ever.
The difficulty now is the time constraints placed on staff and their ability to care for the patient as a person. Equally, these time constraints are having a deleterious effect on the welfare of staff. As challenging as it might be, it’s important that providers do not lose sight of these impacts – which can be best understood from the perspectives of patients and staff themselves.
At Picker, we measure excellence in healthcare provision based on the eight Picker Principles of Person Centred Care:
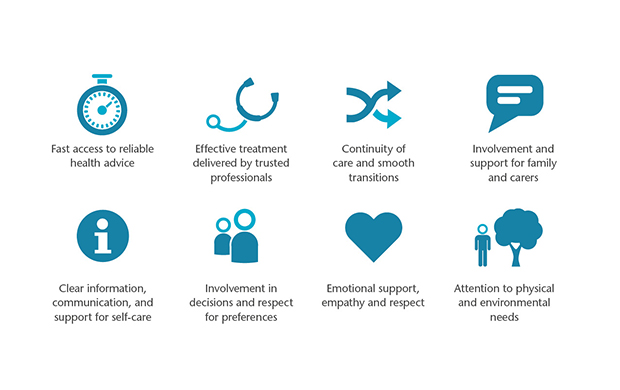
The Picker Principles of Person Centred Care provide a world-renowned framework that outlines the things that matter most to people who use care services. We believe that to deliver high-quality healthcare all these eight principles need to be placed at the heart of healthcare provision.
Clearly, the world has been caught out by COVID-19 and we are grateful simply that our healthcare service is holding up. But each of the Picker Principles still matter. It will be telling when we receive the results from the next round of patient and staff surveys which areas were most lacking. At the moment it’s likely to be the areas that reflect emotional and mental wellbeing.
During crises, the mental health of patients and staff comes under significant pressure. With a focus on clinical outcomes and delivering care, the person behind the role risks being forgotten. This has a lasting impact because as patient experience deteriorates and the healthcare staff’s welfare takes second place, the mental resilience required to cope wanes. The stress of the current situation could leave behind a legacy of mental health issues and related illnesses.
There has been little talk about the known instances where patients have had to leave their families at the door whilst they seek treatment and the lasting impact this lack of emotional support will have. It’s been inevitable that opportunities to keep families together during treatment have been limited. Infection control requires visitors to stay away and the limited supply of PPE doesn’t stretch to patients’ family members.
By approaching patient care during the pandemic with the Picker Principles in mind, we can ensure that key elements that should remain non-negotiable in the delivery of care are included. Therefore, the high-quality care that our NHS strives for will be maintained, the staff will be better able to cope and patient outcomes will be better.

