The importance of questionnaires for patient satisfaction
Questionnaires are regularly used to measure how satisfied people are with a particular service or product. For example, in health and social care, user views on quality are generally explored using questionnaires that ask about people’s experiences of care.
Experience or satisfaction?
Satisfaction is a subjective lens; what is acceptable to one person can be unacceptable to another. Asking patients and service users experience-related questions about specific events during and after their care enables the collection of data through a much more objective lens, ensuring that results are actionable to allow for improvement.
Questionnaires that measure satisfaction are often vague. For example, consider the question ‘Were you satisfied with the information you were given?’. People have varying expectations of information, which will impact how they answer this question. If their response indicates they were not satisfied, it does not indicate which aspect(s) of information they were dissatisfied with. Nor does it tell us why they were dissatisfied: perhaps they received no information, or the information they did receive was hard to understand.
Now consider the questions ‘Did you understand the information given to you about your care and treatment?’, and ‘Did you receive enough information about your care and treatment?’. These questions are more specific and provide a focus for patients’ answers about aspects of information provision.
Person centred care and the Picker Principles
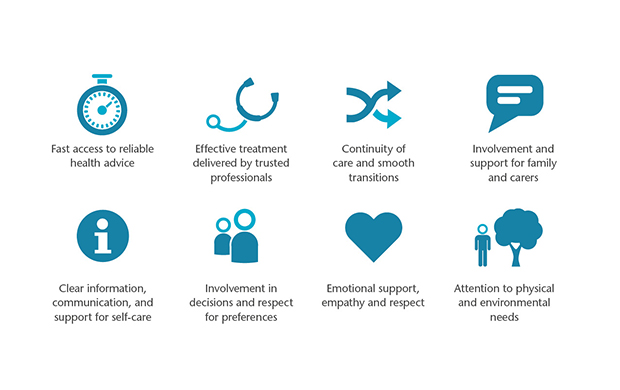
Measuring patient experience through a person centred lens is becoming the industry standard in healthcare research. The Picker Principles underpin elements of person centred care by recognising the importance of the transactional and relational aspects of care.
Incorporating these elements that contribute to a patient’s overall experience of care into a patient questionnaire is essential to ensure it is as person centred as possible.
Patient experience and care quality
In England, policy defines quality in healthcare as a combination of – clinical effectiveness, safety, and people’s experience.
By asking people about their care experiences, we produce actionable data that can be used to support improvements in care quality. In addition, asking about different aspects of care, for example, speed of access to care, information and communication, and involvement in decisions, leads to an objective understanding of where improvement is needed.
There is evidence that a more positive patient experience is associated with better patient safety and effectiveness. Researching and understanding care experiences through a person-centred lens can therefore lead to benefits for the entire healthcare system. For example, understanding and improving information about self-managing a long-term condition can:
- improve the overall experience for patients;
- increase staff confidence and performance in providing information to patients, thus reducing any safety concerns; and
- reduce the likelihood of patients requiring further care (eg hospital readmission or GP care), which reduces overall demand and costs for the healthcare system.
Value of benchmarking
One of the most valuable outputs of questionnaires is the ability to benchmark. Benchmarking allows comparison with previous survey results, between departments or with similar organisations. Engaging in benchmarking allows organisations to monitor progress, identify weaknesses and measure the impact of policy and initiatives by comparing results and identifying trends in patient-reported experience.
Comparing results with similar organisations is incredibly valuable in developing realistic goals and targets for your organisation. Benchmarking can be a disheartening exercise if your results are below average. However, identifying, approaching, and collaborating with organisations that are performing above average can lead to a shared understanding of best practice.
Sharing results and initiatives
Asking the right questions provides insight into areas of good and poor performance, allowing you to target resources, prioritise initiatives and achieve quick wins. Where possible and appropriate, sharing results with patients, and planning initiatives to improve services and user experience is an excellent way to express thanks to survey participants. Additionally, knowing their contribution has influenced change can increase the likelihood that participants will contribute to further research in the future.
Understanding patient experience of care is a continual process that requires ongoing measurement and monitoring to ensure patient needs are met, and that initiatives are making a difference to care.
Further links
Further information on measuring patient satisfaction can be found here.
Examples of good practice in using questionnaires to measure and improve experience:
- The Welsh Ambulance Service Trust translated survey results into tangible outcomes to improve the service they provide.
- The Patient Experience Network (PEN) podcast – University Hospitals Bristol and Weston, discuss using the national Cancer Patient Experience Results to improve patient care.

