Starting your quality improvement journey in an NHS trust
Laura Polkinghorne, Quality Improvement Facilitator at Portsmouth Hospitals University NHS Trust (PHU), talks to us about her role and the positive changes being made to improve staff wellbeing.
Can you tell us about PHU?
At PHU we are proud to deliver safe, compassionate care.
We provide health services for our local population of 675,00 residents across Portsmouth and southeast Hampshire. We also offer specialised treatments to a wider area in excess of two million people.
We offer a full range of outpatient and diagnostic facilities at community sites and local treatment centres across Portsmouth and southeast Hampshire. These include:
- St Mary’s Hospital provides midwifery, dermatology and enablement services.
- Gosport War Memorial Hospital where we offer a range of services including the Blake Maternity Unit, Minor Injuries Unit and diagnostics.
- Petersfield Community Hospital where the Grange Maternity Unit is based.
We have over 7,200 staff, 1,200 beds and an annual turnover close to £600 million. We have 28 operating theatres and, in January 2020, PHU achieved an improved rating of “good” following a comprehensive inspection by the Care Quality Commission (CQC).
In July 2020 we were awarded University Hospital status and have a reputation for award-winning research and development. We work closely with patients, universities, industry and others, using cutting edge science and technology to create real-life tests and treatments that benefit patients more quickly.
Could you tell us a bit about yourself and your role?
I’m a (about to turn 40! Arrrghhh! How did that happen?!) married mum of two boys. My career started in the Royal Navy (RN) as a medical assistant and I went on to train as an operating department practitioner (ODP), a registration I still maintain. I joined the NHS in 2007 as an ODP working in Theatres, where my passion and drive to try to make things better for patients and staff grew.
The anaesthetic consultants and trainees at PHU were always striving to do better and included me in their work. I began to work with other multidisciplinary teams and was learning about the trust as a whole, rather than our one large area.
The trust was on the hunt, seeking colleagues who wanted to be involved in positive change and be a part of the Culture Change programme. The programme is based on the collective leadership model, a three-stage approach: Discovery, Design and Deliver. This programme was developed by NHS Improvement and the King’s Fund and has been successfully piloted in several large acute trusts.
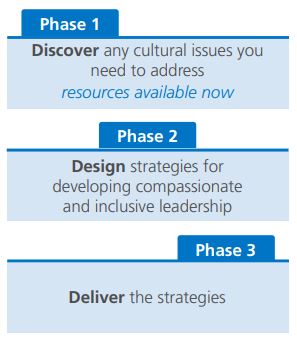
I extended my role as QI Facilitator to include being a Culture Change Agent. As change agents, we are ambassadors and champions for the culture and leadership work, reporting directly to the board. We are currently in Phase 3 of our programme, the “delivery” phase.
I care deeply about PHU, my local hospital where my family and I have been patients. My two sons were born here with the help and compassionate care from the staff. I want to play my part in making it better for my family and my colleagues, their families and our wider communities that includes many veterans and military personnel.
There have been lots of development opportunities as part of this programme, and this has actually opened new doors for my career. Through the programme and learning about quality improvement methodology, I am now a quality improvement facilitator for our trust. I wouldn’t be here doing a job I love if it wasn’t for this programme and having the courage to apply.
How do you collect feedback from staff?
We used a number of sources of information: the NHS Staff Survey and local surveys, the Staff Friends and Family Test (SFFT), CQC reports, meeting reports, face-to-face focus groups, conversations in the workplace and trolley dashes. We decorated a trolley with posters, then filled it with goodies like pens and sweets, and the survey questionnaires. We then visited the majority of areas of the trust, including offsite locations to get feedback from the shop floor staff and anyone wearing a PHU badge. It was really good to be talking to staff and being visible. We also counted the number of staff we had spoken to, to add to our metrics.
What culture change initiatives have you introduced?
So far, following feedback from staff, we have introduced several changes and initiatives:
Leadership behaviours model: after talking to staff, we developed and introduced a living and breathing leadership behaviours model. This will be used for appraisals, when recruiting new members of staff and for current staff development.
Staff Benefits Brochure: this pulls together all the services and offers available for staff in one place. To recognise colleagues’ commitment and dedication, the brochure provides them with benefits and support throughout their careers.
‘Thank you’ cards: to thank those that have gone above and beyond, the change agents implemented ‘Thank you’ cards. Colleagues can send each other a card to show their appreciation to anyone working at the trust.
Induction pack: we have also improved our local induction pack, which is now more relevant and adaptable to the individual department, as well as more welcoming for new starters.
Long-serving staff: to recognise those colleagues who have dedicated a long service to the NHS, we have introduced a new initiative where colleagues receive a long-serving badge and certificate. These have been well received and as a trust shows our appreciation.
The change agents have also influenced:
- The Working Together Strategy.
- The trust’s Communication and Engagement Strategy.
- Values into Action development sessions.
- The Affina Organisational Development Team Coach Journey.
Currently, with a national focus on staff wellbeing, we would like to support the importance and culture of taking rest breaks at work and introduce a wellbeing champion role.
How do you sustain change and maintain enthusiasm for projects?
Change can only happen effectively as a team. It’s about engaging staff with a shared purpose and empowering them to make change happen. It’s important to understand the motivation of teams and individuals, and seeing things from their perspective.
It’s important to include staff, and that also means valuing and understanding their opinions too. Understanding the “why” for staff and patients is a good motivator, especially with stories and facts to show there actually is a problem. Going back to these regularly and getting feedback as change happens means that things can be adapted where necessary along the way.
It’s a continuous journey that isn’t just a one-off fix. Celebrate successes and hard work, but also the learning from things not going to plan. The learning is often more important and when it’s turned around, the most celebrated.
I love working with teams and seeing their improvements, collaboration and confidence grow. That is a success for me.
For more information about quality improvement, please contact Insight@pickereurope.ac.uk

