Improving the experience of men living with prostate cancer
Northampton General Hospital NHS Trust is an accredited cancer centre and provides cancer services to people who live in Northamptonshire and Buckinghamshire. In 2020, it treated 627 men for prostate cancer and was keen to understand their experiences of cancer services.
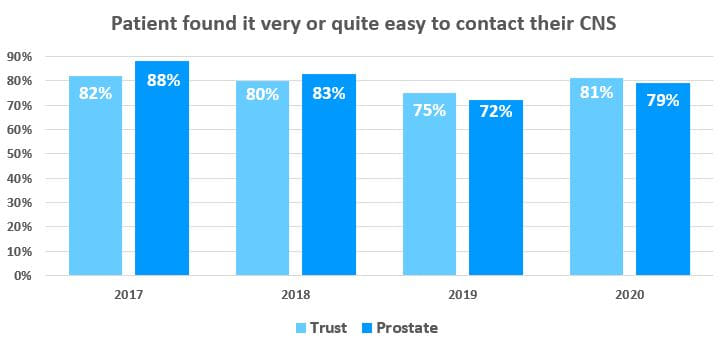
Previous years National Cancer Patient Experience Survey (NCPES) results showed patients were struggling to contact their Clinical Nurse Specialist (CNS), with prostate cancer scoring the lowest. Staff wanted to work with patients to improve this so a working group was created that included: two patients, patient experience leads, urology nurse specialists, a Macmillan cancer lead nurse, a Macmillan Cancer Recovery Package Lead and a Macmillan Patient Information and Support Lead.
Before the project, the unit was staffed by two specialist Macmillan uro-oncology clinical nurse specialists. A further cancer specialist nurse was recruited thanks to the support of PROSTAid.
The healthcare professionals listened to the patients to understand their needs and worked with them to make changes. Patient views were central to the whole project; all change ideas came from men living with prostate cancer, supported by staff.
Challenges
The trust score in the NCPES for patients being able to easily contact their Clinical Nurse Specialist (CNS) was below the expected range and so considered a negative outlier. This score was getting gradually lower, and the team realised they needed help to make measurable improvements. Around the same time, the NHS Cancer Programme was inviting trusts to join its Cancer Experience of Care Improvement Collaborative which provided support with structuring their project within a framework of quality improvement science.
The prostate cancer team collected baseline data from their patients to gain an understanding of the men’s experiences before changes were implemented. The NHS Cancer Programme was able to advise on tracking data to show which changes were creating a measurable and sustainable improvement.
Based on the insights from patients, the team learned that their plans needed to change. They recognised the need to coproduce changes to their service with patients that had lived experience of prostate cancer care within their unit.
Actions
The trust set up a working group led by the Macmillan Cancer Lead Nurse. The aim was to work collaboratively with patients and trial new ways of working to ensure patients had access to the information and support they needed through the cancer pathway. The team met for half an hour every Monday to sustain the momentum.
The working group approached two patients to support the project, one of whom was also the chair of the local prostate cancer support group and the other was also the chair of PROSTAid. This gave the team access to insights from all the men within the support groups, as well as the two main contacts.
Baseline data was provided by several sources: the NCPES survey results, asking patients if it was easy to contact their CNS, and by tracking the number of phone calls answered versus the number that went to voicemail. A patient representative on the team suggested it was also important to understand why a person was contacting the CNS so they could categorise the issues eg feeling unwell, appointment query, etc.
Insight from the team’s data highlighted that some patients with acute medical issues were waiting all day to speak to a CNS when they needed urgent treatment. A telephone triage system was then introduced that filtered patients according to their need, eg medical issue or financial support.
To enable patients to self-manage aspects of their care, the team developed a series of webinars and videos. These also provided information and support for friends and family.
Feedback from patients highlighted that the information given to patients at diagnosis was rarely read. This meant the men didn’t know who to contact for different issues, so the team created a dedicated information sticker that quickly signposted the help available for various scenarios.
Using a driver diagram to plan the improvement activities the team could see which were contributing to positive changes. Then, a Statistical Process Chart (SPC) was used to measure the improvement and understand the variation in change and if it was sustainable.
Impact
The SPC chart illustrated the percentage of calls directly answered by the nurse specialists before the change ideas were implemented. The data demonstrated an improvement from 48% to 93% of calls answered directly, after three months of the project launch in 2020.
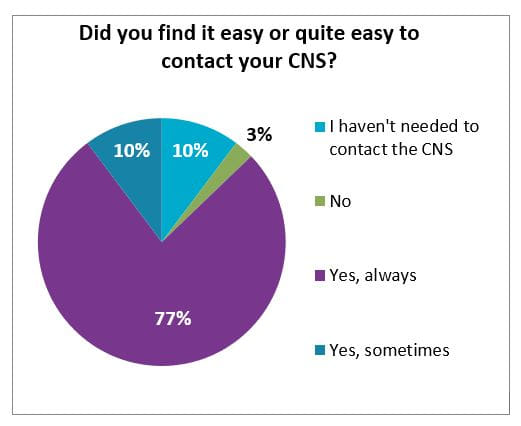
The patient experience team phoned 39 patients after the changes were introduced to understand the impact. The majority of patients (87% vs 45% baseline) said they found it ‘easy’ or ‘quite easy’ to contact their CNS:
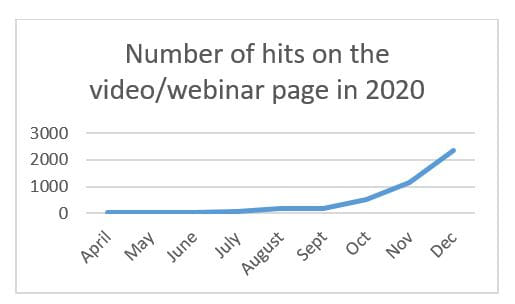
Usage of the self-management videos/webinars showed the number of views since the start of the initiative had risen from 29 to nearly 2,500 in December 2020. Patients were invited to make any comments anonymously after viewing the content, and the data showed a significant improvement in patient experience during 2020.
In the 2019 NCPES survey, 72% of prostate cancer patients said they were easily able to contact their CNS and in 2020 this has risen to 79%.
This work has changed the way cancer healthcare professionals at the trust engage with patients; they have been able to help men living with prostate cancer to self-manage with support through the cancer pathway and move away from traditional models of care. This new way of working will now be rolled out across other tumour sites.
Going Forward
The team are planning to introduce a YouTube channel containing all the webinars and videos that have been created. This will then be extended to include content for all tumour sites.
They have started to run live Q&A sessions for patients, with panellists from specialities such as surgery, oncology and dietetics. The aim of these sessions is to ensure patients can get all their questions answered and aren’t worrying about aspects of their care.
“The National Cancer Patient Experience Survey supported us to make local improvements to cancer care based on what matters most to our patients.”
Elizabeth Summers, Macmillan Cancer Lead Nurse.


