Adult inpatients’ experiences of care – 2019 survey results discussed
The 2019 Adult Inpatient Survey received over 76,000 responses from patients who were discharged in July 2019. Feedback was given – prior to the pandemic – on all areas of care from admission to discharge for 143 NHS acute trusts. The results show patient experience has deteriorated in areas linked to demand on services; a continuation of a downward trend seen in 2018’s results. This highlights the need for a change in strategy to ensure patients receive the high-quality care set out in the NHS Long Term Plan.
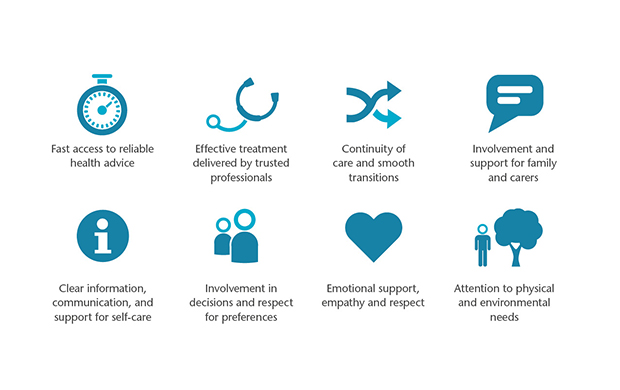
To support the delivery of consistent, high-quality care we use our framework known as The Picker Principles of Person Centred Care. These were developed to outline the things that matter most to people who use care services; key elements of which should remain non-negotiable in the delivery of care. Below we discuss the Inpatient Survey results and how these align with The Picker Principles and the NHS Long Term Plan.
Fast access to reliable healthcare advice
The NHS Long Term Plan intends to reduce the number of emergency admissions by introducing Integrated Care Systems (ICSs). ICSs will deliver urgent care through new avenues such as using Urgent Treatment Centres and by implementing Same Day Emergency Care. Additionally, the Long Term Plan highlights the aim to increase the amount of planned surgery year-on-year, to cut long waits, and reduce the waiting list. However, the 2019 results show emergency admissions are still increasing, with 71% of patients being admitted as an emergency, this is a significant increase from 2018 and is nine percentage points higher than reported in 2010. Furthermore, planned admissions have significantly decreased from 2018, with 25% of patient’s admission being planned, down 2% from 2018 and 9% from 2010.
It is anticipated that through providing more avenues for patients to receive the care they need, the number of beds available will increase. When patients were asked whether they felt they had to wait a long time to get a bed on a ward, 42% of patients said ‘yes, definitely’ or ‘yes, to some extent’, this is a significant rise from 39% in 2018. While policies have been reformed to improve these areas of care, more is needed to ensure this translates into a better patient experience.
Emotional support, empathy and respect
This is an area of care which continues to perform well. The results show some significant changes this year, with fewer patients reporting that doctors and nurses are talking in front of patients as if they weren’t there and more patients ‘definitely’ being given enough privacy while in the A&E department. Additionally, positive trends have been identified in the respect given to patients; 81% of patients feel they are ‘always’ treated with respect and dignity while in hospital.
Involvement in decisions and respect for patient’s preferences
The NHS Long Term Plan has emphasised the importance of engaging patients in decisions about their health and wellbeing to ensure person centred care is delivered. Improvements have been observed in this area, with 55% of patients saying they were ‘definitely’ involved as much as they wanted to be in decisions about their care and treatment. This is a significant increase from 54% reported in 2018 and is four percentage points higher than reported ten years ago. While there is more work to be done in this area through continued support and training for staff, this is a positive result this year.
Continuity of care and smooth transitions
Within the new strategy, the NHS outlines the policy to improve the performance of getting people home without unnecessary delay. The proportion of patients reporting a delay at discharge has remained consistent over the past years, with 41% experiencing a delay. In 2019, there was an increase in the length of the delay, with a smaller proportion of patients reporting the delay was up to 1 hour. 71% of patients recorded the main reason for this delay was due to having to wait for medicines. Further, we have also seen a decrease in the information provided to patients regarding their medicines, discussed further below, which could be as a result of these delays.
Clear information, communication and support for self-care
Finally, as mentioned above, the 2019 results displayed a drop in the information and communication provided to patients with regards to their medication. An increased number of patients said the purpose of their medicines were not explained in a way they could understand, while 44% of patients reported staff did not tell them about the medication side effects.
Overall, the 2019 Adult Inpatient Survey showed that improvements have taken place in terms of shared decision-making and emotional support and respect, but also that negative trends can be observed concerning emergency admissions, discharge and information provision regarding medication. While there are areas of adult inpatient care that do perform consistently well, there are clearly further improvements needed to ensure the delivery of patient centred care. The Picker Principles highlight these areas and ensure people are placed at the heart of healthcare provision.

